Infectious Disease cases evolve with cultures, sensitivities, exposures, and response to therapy. The clinical picture changes as data arrives. Documentation needs to keep pace with that movement.
Infectious Disease cases evolve with cultures, sensitivities, exposures, and response to therapy. The clinical picture changes as data arrives. Documentation needs to keep pace with that movement.
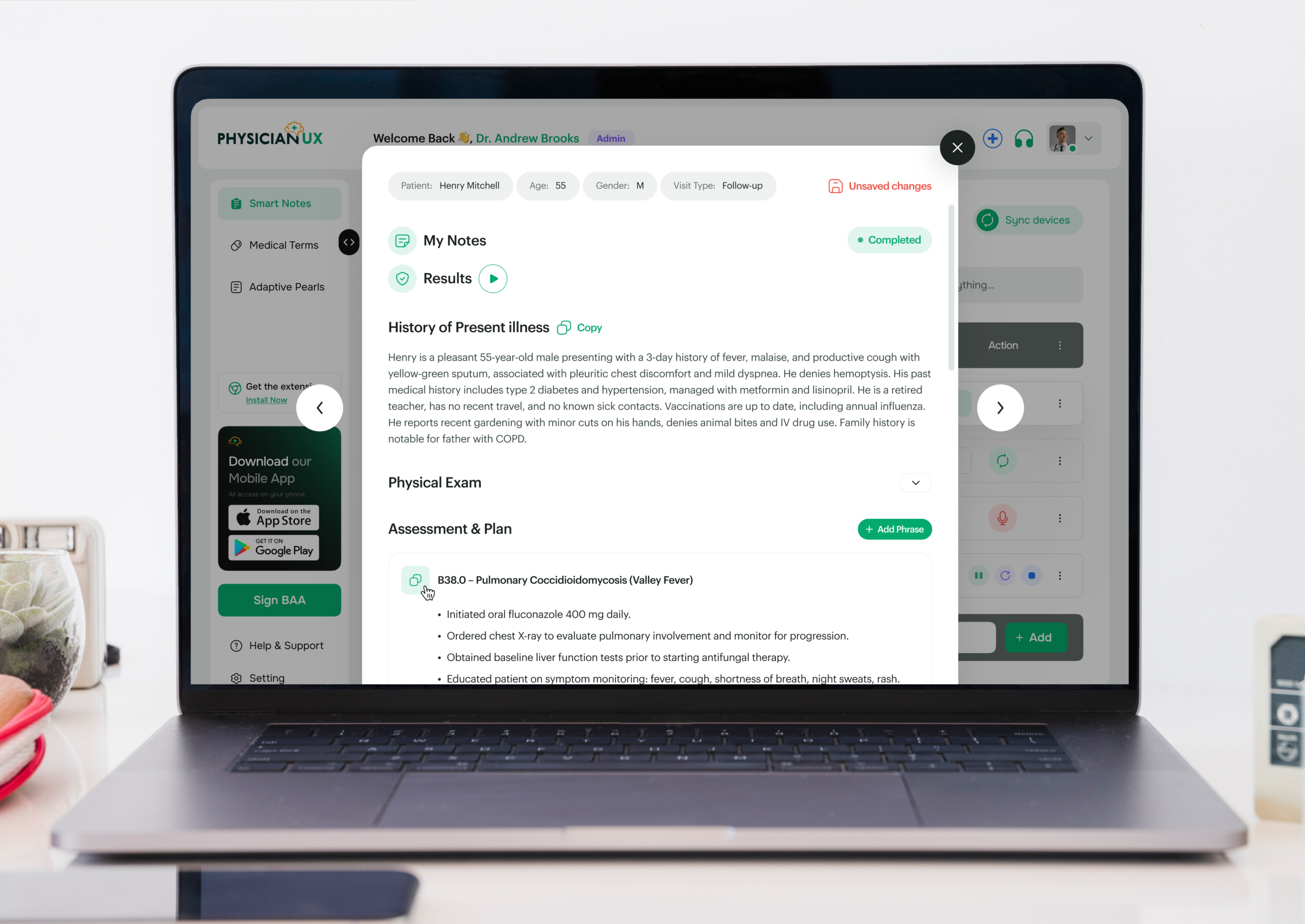
Infectious Disease care evolves continuously — exposures, cultures, sensitivities, imaging, and clinical response all shape decisions over time. Management rarely follows a straight line, and documentation must adapt as new data emerges. Physician UX was designed to follow this reasoning, capturing clinical conversations and producing notes that reflect how infectious disease specialists actually think and manage care.
If you practice Infectious Disease, you know that notes often take longer than the patient encounter. Visits typically involve reviewing extensive labs and cultures, tracking antimicrobial therapy, coordinating with multiple teams, and counseling patients — all while documentation requirements remain detailed, accurate, and legally essential.
You’re capturing:
All while maintaining accuracy and continuity — something no rigid template can fully support.
Infectious Disease visits often require integrating multiple data points, reviewing past treatment responses, and planning complex therapy regimens. By the time you reconcile labs, adjust medications, and document care plans, the next patient is already waiting.
The cognitive load is high. Missed details can impact safety, adherence, and clinical outcomes. When documentation extends beyond clinic hours, burnout intensifies.
Physician UX lifts the documentation burden — without interrupting your workflow. It listens and structures notes in real time, supporting the complex rhythm of Infectious Disease care.
Dr. Nguyen, an Infectious Disease physician, begins her day with multiple patient visits: new HIV consults, multi-drug resistant infections, post-surgical infections, and chronic infection management.
Typically, she would be mentally juggling lab interpretations, antimicrobial adjustments, patient counseling, and care coordination — all while maintaining attention to each patient.
Today, Physician UX is listening in the background.
During her first visit, the platform structures a detailed HPI capturing exposure history, symptom progression, labs, and medication adherence. By the end of the conversation, her note already includes an aligned assessment and plan — complete with tasks queued for follow-up labs, imaging, and therapy monitoring.
Her next patient requires complex antimicrobial management. Physician UX identifies key elements, surfaces pearls for therapy adjustments, and organizes tasks — all without slowing the bedside encounter.
By mid-morning, Dr. Nguyen notices something unusual: she is fully present with patients, not mentally reconstructing notes between visits.
Documentation that would normally spill into evenings is already complete. Tasks are organized, follow-ups mapped, and the burden of manual charting lifted. She can now focus on infection control, therapy decisions, and patient education.
What used to feel like constant triage now feels like practicing Infectious Disease medicine at her full capacity.
When charting becomes lighter and less intrusive, patient care transforms. Physician UX ensures notes are accurate, timely, and aligned with best practices — freeing cognitive bandwidth for complex diagnostic reasoning and patient-centered care.
Better notes also mean safer care:
In a specialty defined by complexity, evolving evidence, and patient safety, clarity isn’t optional — it’s essential.
Join the clinicians who’ve upgraded their workflow — and feel the difference for yourself.