Hospitalists think in real time — coordinating teams, reassessing daily, planning safe transitions. The work is dynamic, but documentation is often static. That mismatch adds unnecessary cognitive load.
Hospitalists think in real time — coordinating teams, reassessing daily, planning safe transitions. The work is dynamic, but documentation is often static. That mismatch adds unnecessary cognitive load.
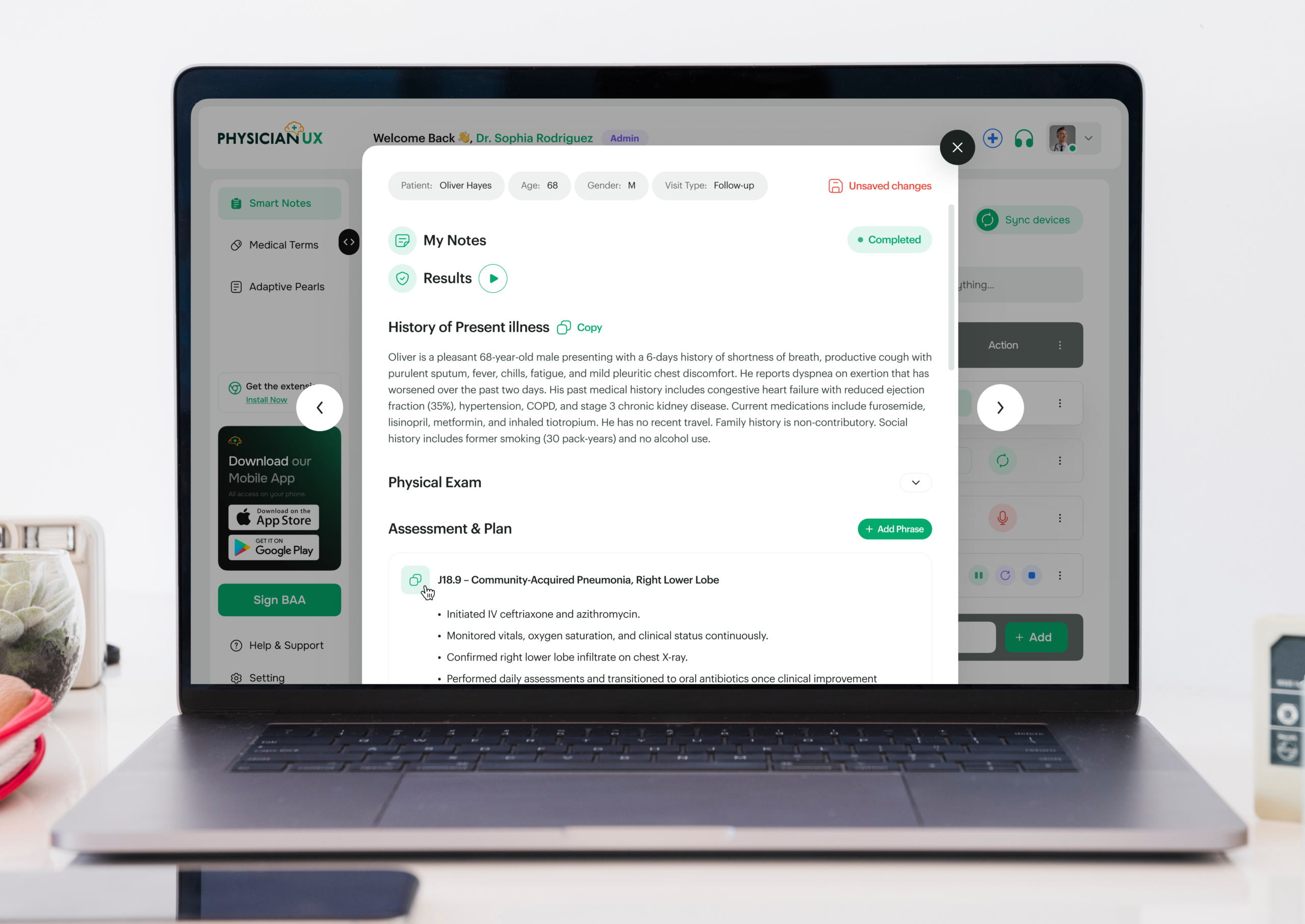
Hospital medicine is practiced in real time — coordinating teams, reassessing patients daily, and managing evolving clinical conditions while planning safe transitions of care. Each decision builds on the last, often across multiple services. Physician UX was designed to support this environment, capturing clinical conversations and producing notes that reflect how hospitalists actually think and manage care moment to moment.
If you practice as a Hospitalist, you know the pressure: patients are often acutely ill, conditions evolve rapidly, and documentation requirements are extensive and legally essential. Every note must reflect complex decision-making while maintaining accuracy and continuity.
You’re capturing:
All while managing high patient volumes and rapidly changing clinical priorities — something no rigid template can fully support.
Hospitalist days often involve juggling multiple admissions, discharges, and complex clinical scenarios simultaneously. By the time you document labs, write progress notes, coordinate care, and prepare discharge summaries, the next patient is already calling for attention.
It’s not just time-consuming — the cognitive load is intense. Missed details can affect safety, continuity, compliance, and communication. When charting spills into evenings, burnout accelerates.
Physician UX was designed to lift the documentation burden — without interrupting your workflow. It listens and structures notes in real time, supporting the dynamic rhythm of Hospital Medicine.
Dr. Lee, a hospitalist in a busy inpatient service, begins her day with multiple admissions, ICU transfers, and a full board of patients requiring daily progress notes.
Typically, she would be mentally juggling lab reviews, imaging results, medication adjustments, consult recommendations, and family discussions — all while trying to stay on top of evolving patient statuses.
Today, Physician UX is listening in the background.
During her first admission, the platform structures a detailed HPI and hospital course based on vitals, labs, imaging, and patient history. By the end of the conversation, her note already includes an aligned assessment and plan — complete with tasks queued for labs, imaging, consults, and follow-ups.
Her second patient requires rapid intervention due to a change in clinical status. Physician UX identifies clinically important elements, surfaces pearls for evidence-based management, and organizes tasks — all without slowing the bedside encounter.
By mid-morning, Dr. Lee notices something rare: she is fully present with each patient instead of reconstructing notes in her mind between rooms.
Documentation that would normally spill into evenings is already complete. Tasks are organized, follow-ups mapped, and the burden of manual charting lifted. She can focus on patient care, team coordination, and complex clinical reasoning.
What used to feel like constant triage now feels like fully practicing Hospital Medicine.
When charting is lighter and less intrusive, hospital care transforms. Physician UX ensures progress notes, admissions, and discharge summaries are accurate and timely — freeing cognitive bandwidth for acute decision-making and patient safety.
Better notes also mean safer care:
In a specialty defined by high acuity, complexity, and coordination, clarity isn’t optional — it’s essential.
Join the clinicians who’ve upgraded their workflow — and feel the difference for yourself.