Geriatrics requires balancing medical complexity with function, cognition, safety, and support systems. Small details change outcomes. Documentation has to carry that weight without adding friction.
Geriatrics requires balancing medical complexity with function, cognition, safety, and support systems. Small details change outcomes. Documentation has to carry that weight without adding friction.
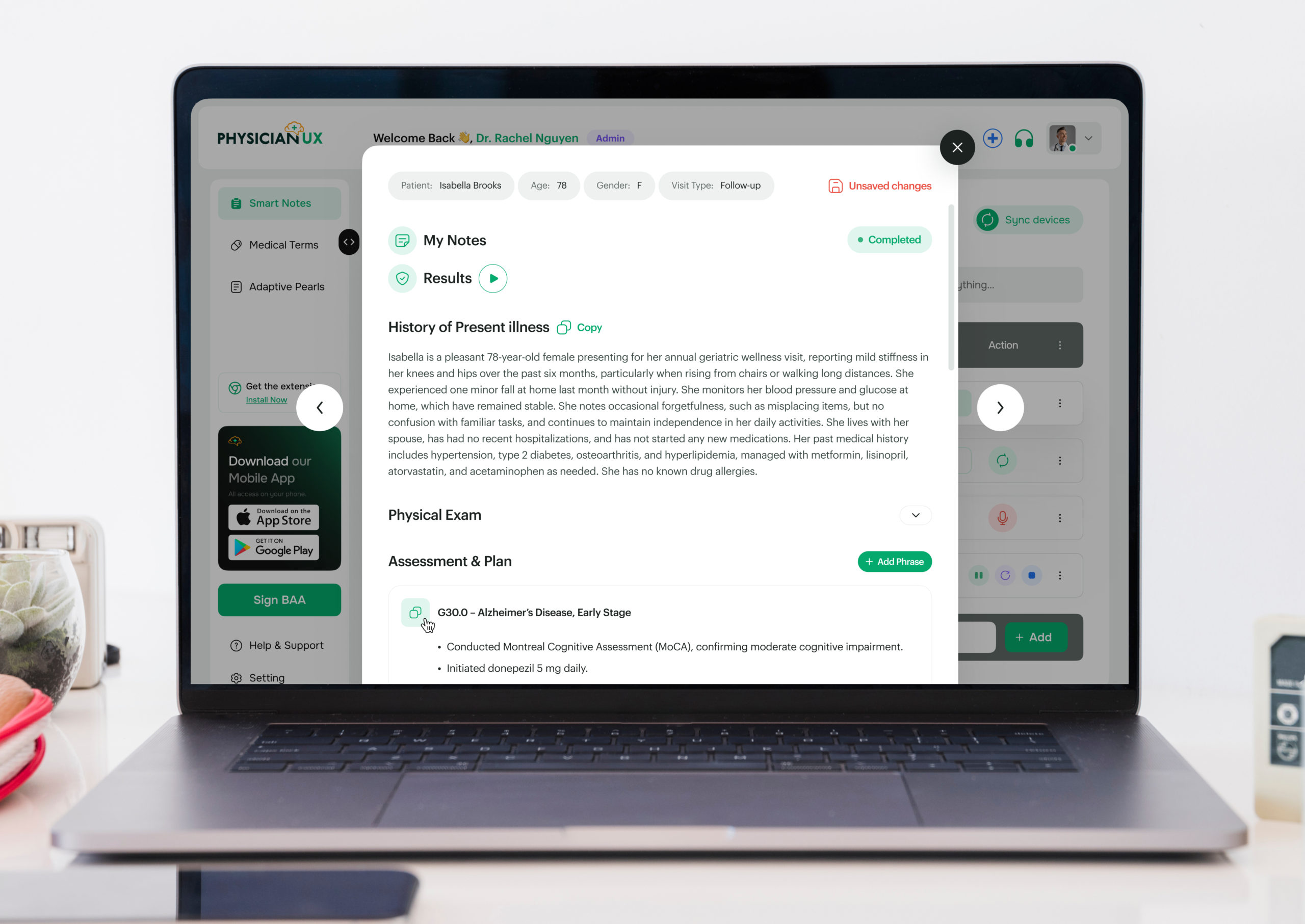
Geriatric care is shaped by complexity — multiple chronic conditions, cognitive and functional changes, medications, and social context all intersect at every visit. Decisions are rarely isolated and often evolve over time. Physician UX was designed to support that reality, capturing clinical conversations and producing notes that reflect how geriatric clinicians actually reason and plan care.
If you practice Geriatrics, you already know the challenge: visits often take longer than the allotted time, and documentation can be overwhelming. Patient conversations are multifaceted, often covering polypharmacy, chronic disease management, functional assessments, and caregiver concerns — while notes must remain thorough, compliant, and clinically defensible.
You’re capturing:
All while maintaining patient-centered care, dignity, and continuity — something no rigid template can fully support.
Visits often address multiple organ systems and social factors. By the time you review medications, lab trends, functional assessments, and care plans, the next patient is already waiting.
It’s not just time-consuming — the cognitive load is heavy. Missed details can affect safety, continuity, compliance, and coordination. When charting extends into evenings, clinician fatigue accelerates.
Physician UX was designed to lift the documentation burden — without interrupting your workflow. It listens and structures notes in real time, supporting the natural rhythm of Geriatrics.
Dr. Thompson, a geriatrician in a busy outpatient clinic, begins her day with six consecutive visits: chronic disease follow-ups, cognitive assessments, functional evaluations, and complex patients balancing multiple medications and caregiver needs.
Typically, she would be mentally juggling polypharmacy, lab trends, cognitive evaluations, functional assessments, and caregiver communication — all while remaining attentive to each patient.
Today, Physician UX is listening in the background.
During her first visit, the platform structures a detailed HPI capturing functional status, cognitive changes, medication adherence, and social support. By the end of the conversation, her note already includes a structured assessment and plan — complete with tasks queued for labs, medication adjustments, and follow-ups.
Her second patient presents with mobility concerns and mild cognitive changes. Physician UX identifies clinically important elements, surfaces pearls related to fall prevention, medication review, and functional interventions — all without slowing the encounter.
By mid-morning, Dr. Thompson notices something new: she’s fully present, thinking clearly, and not mentally reconstructing notes for each patient.
Notes are complete as visits conclude. Tasks are organized, follow-ups mapped, and the burden of manual documentation lifted. She can focus on complex geriatric care and patient-centered discussions.
What used to feel like survival mode now feels like practicing medicine again.
When charting becomes lighter and less intrusive, the clinical encounter transforms. In Geriatrics — where chronic disease, functional status, cognition, and social context intersect — freeing cognitive bandwidth directly improves care.
You can stay fully present without splitting attention between typing, tracking labs, adjusting medications, or coordinating care.
Better notes also mean safer care:
In a specialty defined by complexity, frailty, and continuity, clarity isn’t optional — it’s essential.
Join the clinicians who’ve upgraded their workflow — and feel the difference for yourself.