Built for the Reality of Nutrition Counseling
Nutrition care is built on conversation, behavior change, and trust developed over time. Each visit adds nuance, context, and motivation — yet most documentation tools reduce these interactions to rigid templates. Physician UX was designed to support how dietitians and nutritionists actually work, bringing structure to complex counseling without disrupting flow or patient connection.
The Documentation Overload in Nutrition Practice
If you work in nutrition care, you already know that the note often requires just as much attention as the consultation. Your visits are holistic by nature — exploring food patterns, emotions, lifestyle barriers, medical comorbidities, and real-world challenges that shape behavior change.
You’re documenting detailed elements such as:
- 24-hour recalls, food frequency patterns, macronutrient breakdowns, and dietary trends
- Motivational interviewing for readiness, ambivalence, and goals
- Nutrition-specific vitals: weight history, body composition, anthropometrics
- Meal planning discussions and practical modifications
- Comorbidities such as diabetes, CKD, heart disease, GI disorders, and malnutrition
- Behavioral, cultural, and socioeconomic contributors to eating habits
- Care coordination with PCPs, endocrinology, gastroenterology, or bariatrics
All this happens in a conversation that isn’t linear — patients jump between questions, concerns, emotions, and insights. Traditional templates simply can’t keep up.
Charting becomes especially heavy during initial assessments, complex chronic-disease visits, pediatric consultations, and multidisciplinary care plans. By the time you finish documenting behavioral strategies, SMART goals, barriers, meal timing, and follow-up recommendations, you’re already behind schedule.
The cognitive load adds up: recalling measurements, tracking long-term progress, adjusting treatment plans, and documenting key nutrition markers. And when it spills into the evening, burnout isn’t far behind.
How Physician UX Supports Nutrition Care
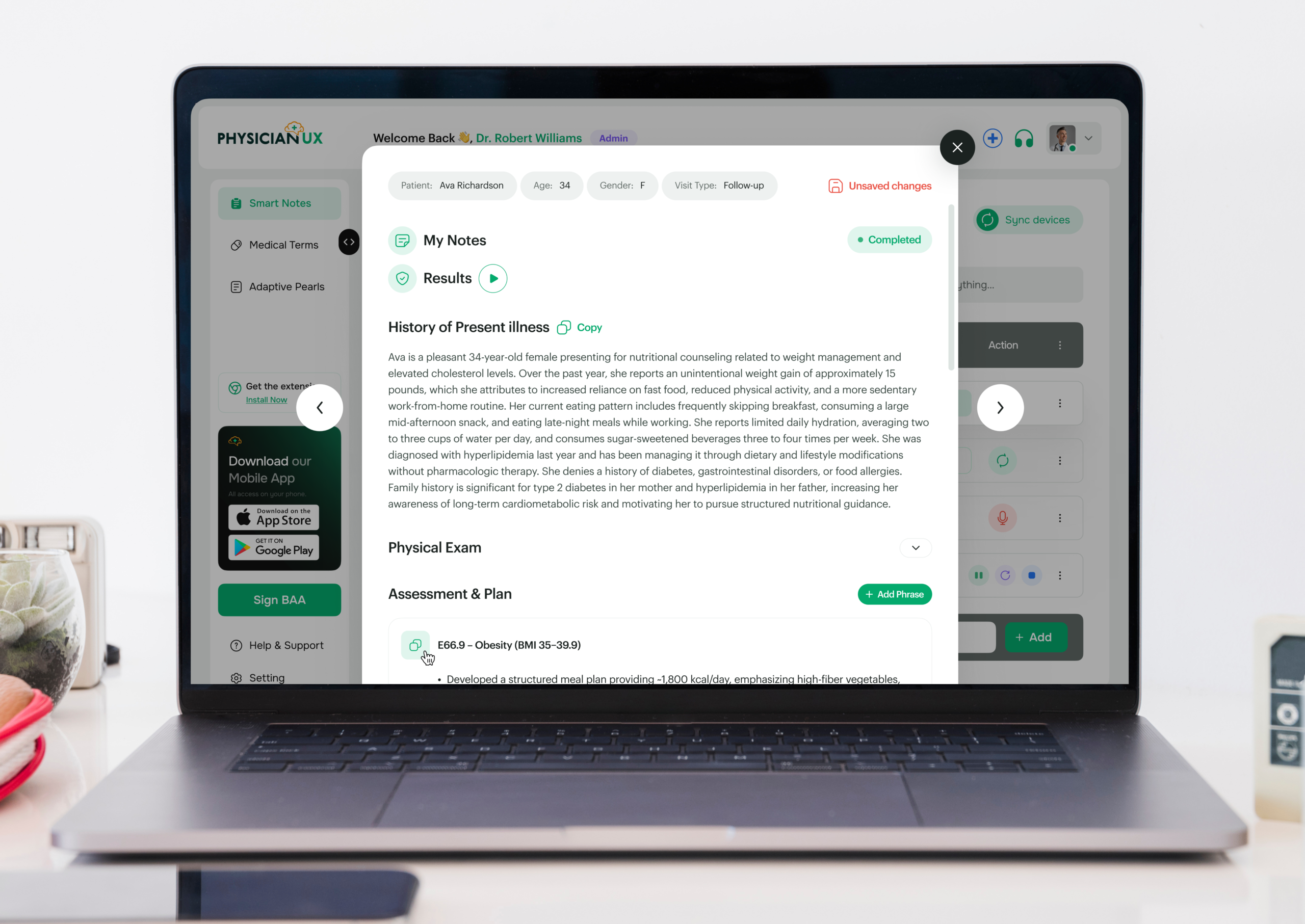
Physician UX brings structure to counseling without breaking the flow of conversation — so documentation becomes lighter, more precise, and more clinically useful.
- Automatic visit capture that organizes dietary history, patient motivations, barriers to change, and nutrition-related symptoms.
- Specialty-tuned nutrition SOAP notes aligned with evidence-based frameworks used in clinical dietetics: ADIME, SMART goals, behavior-change strategies, and disease-specific guidelines.
- Context-aware Clinical Pearls surfaced in real time — from carbohydrate counting reminders to CKD protein guidance, IBS modifications, allergy considerations, and malnutrition criteria.
- Smart Phrases for meal planning, lifestyle counseling, chronic disease management, pediatric growth counseling, motivational interviewing, and follow-up instructions.
- Automatic task generation for follow-up measurements, lab checks, interdisciplinary coordination, referrals, and patient education reminders.
- Organized continuity tools that track goals, anthropometrics, and longitudinal nutrition markers across visits.
- Reduced cognitive load, helping you stay fully present during emotionally and behaviorally complex conversations.
A Day in Nutrition Practice, Reimagined
How Counseling Flows More Naturally When the Note Writes Itself
Sarah, a registered dietitian working in an outpatient metabolic clinic, begins a full schedule: new diabetes consults, weight-management follow-ups, a CKD patient struggling with protein targets, and two pediatric feeding concerns.
Normally, she would spend the entire morning juggling food recall details, medication interactions, growth curves, and motivational interviewing notes — all while trying to guide patients through realistic habit changes.
But today, Physician UX is quietly listening.
As she walks through a patient’s dietary recall, the platform structures the HPI around timing, portions, macronutrient patterns, hunger cues, and barriers such as stress or schedule constraints. The note is already forming — naturally, without forcing her into rigid boxes.
Her next patient is a teen with IBS. As she gathers information about triggers, food avoidance, GI symptoms, and stress patterns, Physician UX surfaces pearls about low-FODMAP considerations and red-flag symptoms. It organizes everything into a clean, clinically accurate SOAP note.
For the first time in a long time, she notices she isn’t “remembering things for later.” Everything is already captured, clearly and accurately.
By midday, meal-plan adjustments, progress markers, anthropometric measurements, and follow-up tasks are all documented. No backlog. No mental overflow. She’s fully present and able to give each patient attention without worrying about falling behind.
And when her last patient leaves, her documentation is already complete — not waiting for her hours later at home.
Better Documentation → Better Nutrition Outcomes
When charting becomes lighter, dietitians gain the space needed to truly connect with patients — to explore motivations, clarify goals, and offer personalized strategies that stick.
Clearer notes translate into better care:
- More accurate tracking of weight trends, labs, and nutrition markers
- Better follow-through on SMART goals and behavior change strategies
- Improved coordination with referring clinicians and multidisciplinary teams
- Early identification of clinical red flags or nutrition risks
- More time for education, shared decision-making, and practical planning
Nutrition care is deeply human — and when documentation supports rather than interferes, patients feel the difference immediately.