GI care spans symptoms, procedures, pathology, imaging, and evolving treatment plans. The story rarely fits into one visit or one system. Capturing that continuity is where documentation usually breaks down.
GI care spans symptoms, procedures, pathology, imaging, and evolving treatment plans. The story rarely fits into one visit or one system. Capturing that continuity is where documentation usually breaks down.
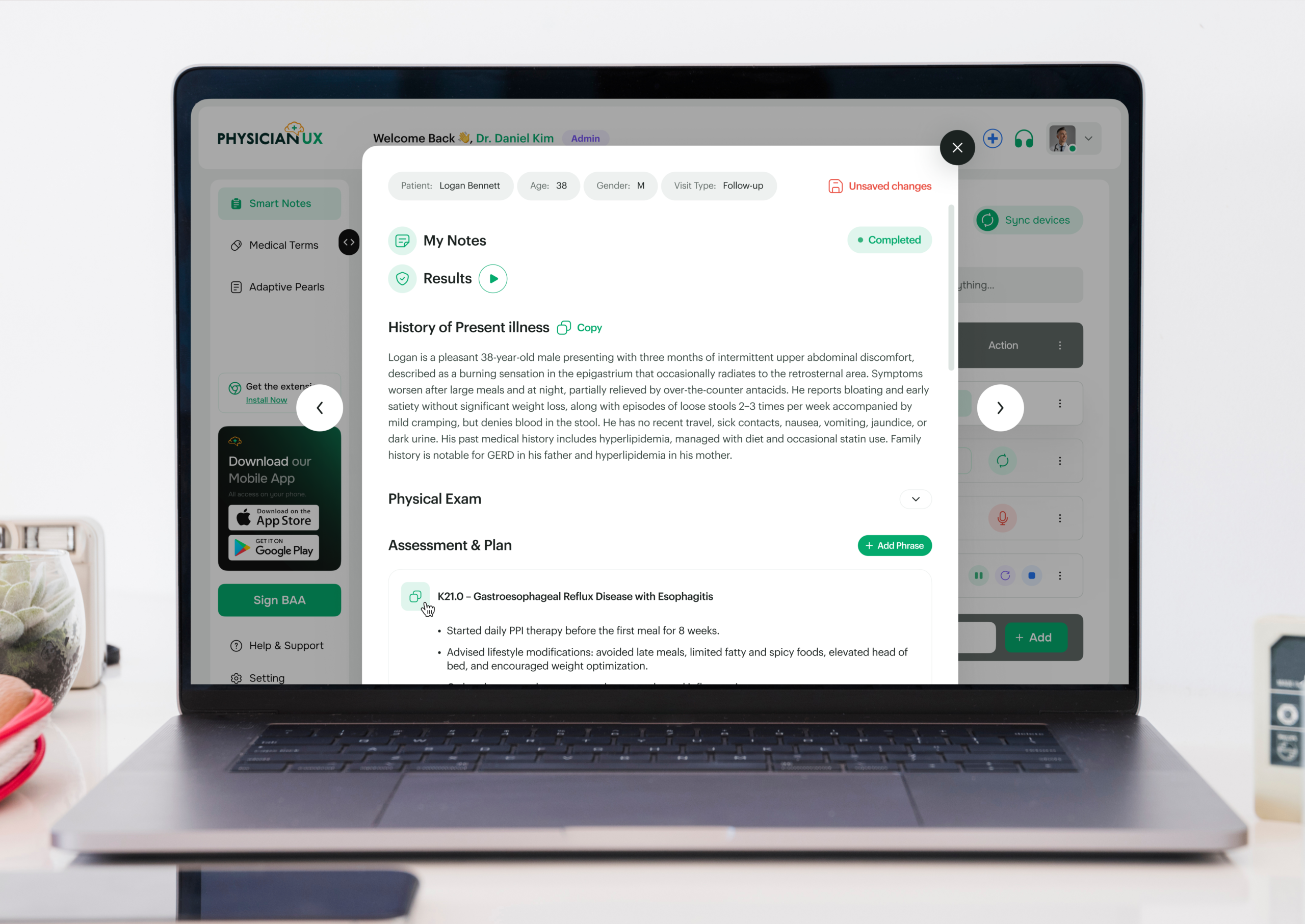
Gastroenterology spans functional disorders, chronic disease, procedures, and long-term management. Clinical reasoning unfolds across symptoms, labs, imaging, pathology, and follow-up — yet most documentation tools treat GI care as a single-visit snapshot. Physician UX was designed to follow that reasoning, capturing conversations and producing notes that reflect how gastroenterologists actually think and manage care.
If you practice Gastroenterology, you already know the challenge: notes often take longer than the visit itself. Patient histories can be complex, spanning chronic liver disease, inflammatory bowel disease, functional GI disorders, and acute presentations — while documentation must remain detailed, compliant, and clinically accurate.
You’re capturing:
All while maintaining continuity of care and addressing patient concerns — something no rigid template can fully support.
Visits often involve multiple problems in one encounter. By the time you review labs, imaging, document procedures, and schedule follow-ups, the next patient is already waiting.
It’s not just time-consuming — the cognitive load is heavy. Missed details can affect patient safety, continuity, compliance, and coordination with interdisciplinary teams. When charting spills into evenings, burnout accelerates.
Physician UX was designed to lift the documentation burden — without interrupting your workflow. It listens and structures notes in real time, supporting the natural rhythm of Gastroenterology.
Dr. Lee, a gastroenterologist in a busy outpatient practice, begins her day with six consecutive visits: an IBD follow-up, liver disease management, colonoscopy prep review, acute abdominal pain, and two patients with chronic reflux.
Typically, she would be mentally juggling lab results, imaging findings, medication adjustments, dietary counseling, and procedural planning — all while remaining attentive to each patient.
Today, Physician UX is listening in the background.
During her first visit, the platform structures a detailed HPI capturing symptom patterns, medication adherence, diet, and lab trends. By the end of the conversation, her note already includes a structured assessment and plan — complete with follow-up tasks and procedure reminders.
Her next patient presents with acute abdominal pain. Physician UX identifies clinically important elements, surfaces relevant pearls for differential diagnosis, and aligns follow-up labs and imaging — without slowing the visit or forcing rigid templates.
By mid-morning, Dr. Lee notices something unusual: she’s fully present, not mentally backtracking through charting details. Her cognitive load has lifted.
Notes are complete as visits conclude. Tasks are organized, follow-ups mapped, and the burden of manual documentation has lifted. She can now focus on complex clinical decision-making and patient counseling.
What used to feel like survival mode now feels like practicing medicine at the top of her ability.
When charting becomes lighter and less intrusive, the clinical encounter transforms. In Gastroenterology — where chronic disease management, procedural planning, and acute complaints intersect — freeing cognitive bandwidth directly improves patient care.
You can stay fully present without splitting attention between typing, tracking labs, adjusting medications, or planning follow-up tasks.
Better notes also mean safer care:
In a specialty defined by complexity and chronic management, clarity isn’t optional — it’s essential.
Join the clinicians who’ve upgraded their workflow — and feel the difference for yourself.