Built for the Precision and Flow of Audiology Care
Audiology depends on subtle findings, careful histories, and how patients describe changes over time. Those details guide diagnosis, counseling, and long-term management — yet they’re often the first to be lost in rigid documentation templates. Physician UX was designed to follow the natural flow of audiology encounters, capturing conversations and producing notes that reflect how audiologists actually think and practice.
The Documentation Weight in Modern Audiology
If you practice Audiology, you already know how documentation often drags behind the pace of your clinical work. Visits mix technical diagnostics, patient counseling, device management, and long-term auditory rehabilitation — none of which follow a tidy script.
You’re capturing:
- Hearing loss histories, noise exposure patterns, and communication challenges
- Detailed audiograms, tympanometry, OAEs, speech discrimination scores, and thresholds
- Vestibular symptoms, balance concerns, and triggers
- Hearing aid fittings, troubleshooting, real-ear measurements, and device adjustments
- Cochlear implant evaluations, mapping discussions, and expectations counseling
- Family input, environmental factors, and communication strategies
Every encounter blends technical data with deep, personalized education. Even a simple follow-up often requires a multi-layered note — audiometric interpretation, device programming, patient feedback, communication goals, and next steps.
And because many patients are older adults, children, or medically complex, small missed details can affect diagnoses, device choices, and long-term outcomes.
Over time, the administrative load stacks up — hearing aid documentation, compliance paperwork, reports for ENT, school systems, and primary care providers. Inevitably, charting spills after hours.
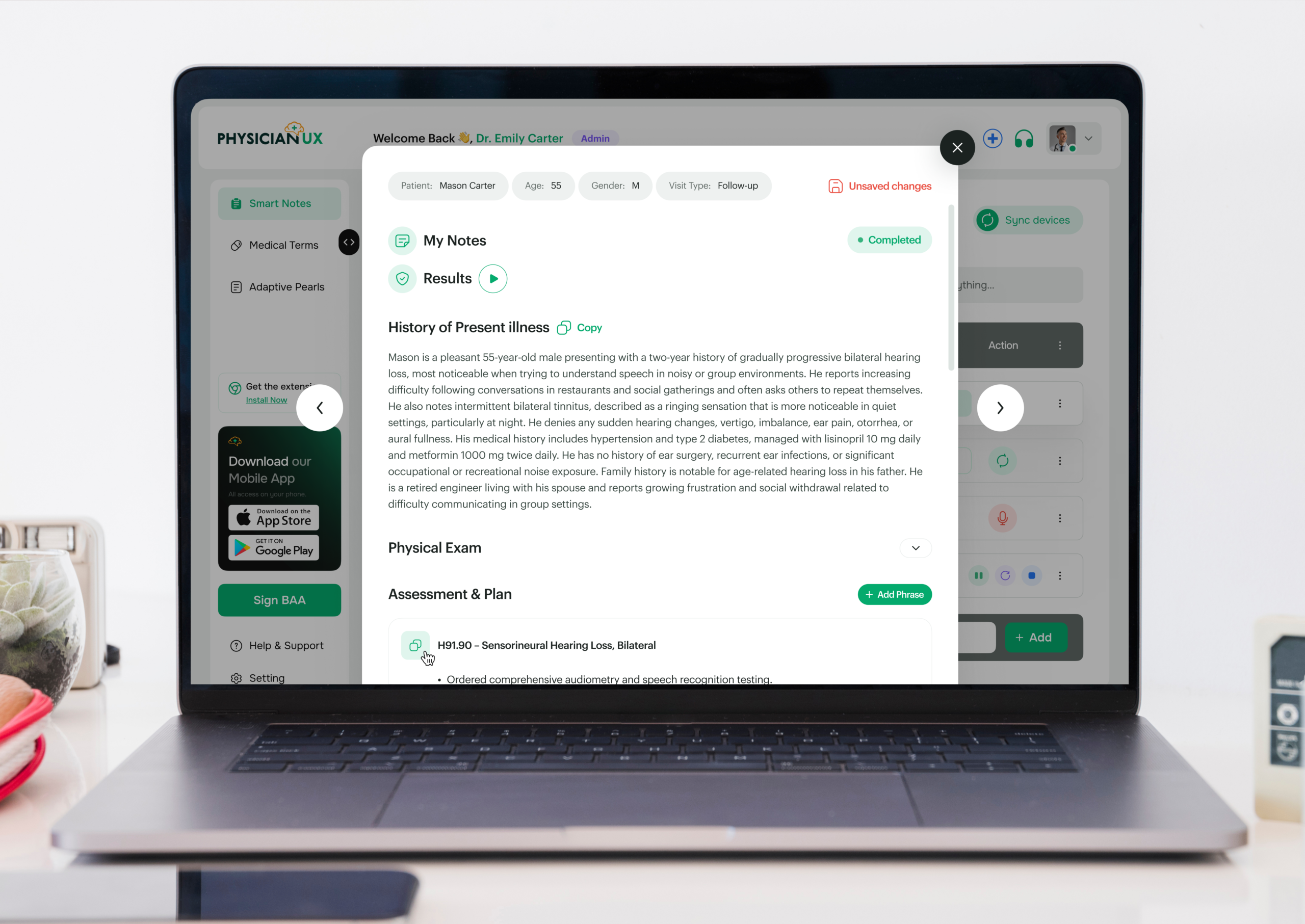
How Physician UX Fits Into Your Workflow
Physician UX supports the real rhythm of Audiology — capturing your clinical narrative naturally, then transforming it into a structured, accurate note that reflects both the diagnostic and rehabilitative aspects of your work.
- Automatic visit capture tuned to hearing loss discussions, tinnitus patterns, vertigo symptoms, device troubleshooting, and counseling flow.
- Specialty-tuned SOAP notes that adapt to audiometric data, hearing aid fittings, vestibular evaluations, and pediatric versus adult encounters.
- Context-aware Clinical Pearls such as differential cues for SNHL vs. conductive loss, vestibular red flags, counseling frameworks, and device optimization considerations.
- Smart Phrases for hearing aid programming, tinnitus counseling, pediatric auditory milestones, cochlear implant pathways, and communication strategy education.
- Automatic task generation for follow-up audiograms, device checks, ENT referrals, tympanometry repeats, CI consults, and hearing rehabilitation planning.
- Clear referral summaries for ENT, neurology, primary care, schools, or speech therapy — improving continuity across teams.
- Reduced cognitive load so your attention stays on patient communication — not catching up on notes.
A Day in Clinic, Rebuilt Around You
How an Audiologist’s Morning Becomes More Efficient
Dr. Avery starts her day with a tinnitus consult, a pediatric hearing evaluation, and two hearing aid follow-ups. Each requires completely different clinical thinking — and completely different documentation.
Normally she’d be toggling between audiograms, device settings, counseling notes, and test interpretation, all while trying to maintain rapport with patients who rely heavily on clear communication.
Today, Physician UX is listening quietly in the background.
During the tinnitus visit, it captures onset patterns, sound qualities, sleep impact, hearing changes, noise exposure history, TMJ factors, and emotional burden — automatically generating a structured history and aligned plan with ENT tasks already queued.
The pediatric evaluation is equally streamlined. It documents developmental milestones, school concerns, parental observations, tympanometry findings, speech detection responses, and the audiogram interpretation — all organized clearly without her typing a word.
By mid-morning, she realizes she’s ahead — something that hasn’t happened in years. Notes are done, tasks are organized, and her mental bandwidth is finally centered on patient connection.
Her hearing aid follow-ups finish with complete documentation, including device adjustments, real-ear measurements, counseling summaries, and troubleshooting steps. No lingering charts. No backlog waiting for lunch or after hours.
Streamlined Documentation → Stronger Hearing Outcomes
Audiology outcomes rely on consistency, clarity, and patient-centered counseling. When documentation becomes lighter and more accurate, the clinical encounter becomes more effective.
Clearer notes support:
- More accurate tracking of hearing thresholds and device performance over time
- Stronger communication with ENT, neurology, and speech-language colleagues
- More consistent follow-up intervals and rehabilitation plans
- Better troubleshooting and device optimization
- Improved adherence to hearing strategies and therapy recommendations
When the cognitive load of charting decreases, you gain time to focus on what truly matters: helping patients reconnect with communication, independence, and confidence.