Neurology often hinges on subtle findings, evolving symptoms, and longitudinal observation. What’s absent can matter as much as what’s present. Documentation must capture that level of thinking.
Neurology often hinges on subtle findings, evolving symptoms, and longitudinal observation. What’s absent can matter as much as what’s present. Documentation must capture that level of thinking.
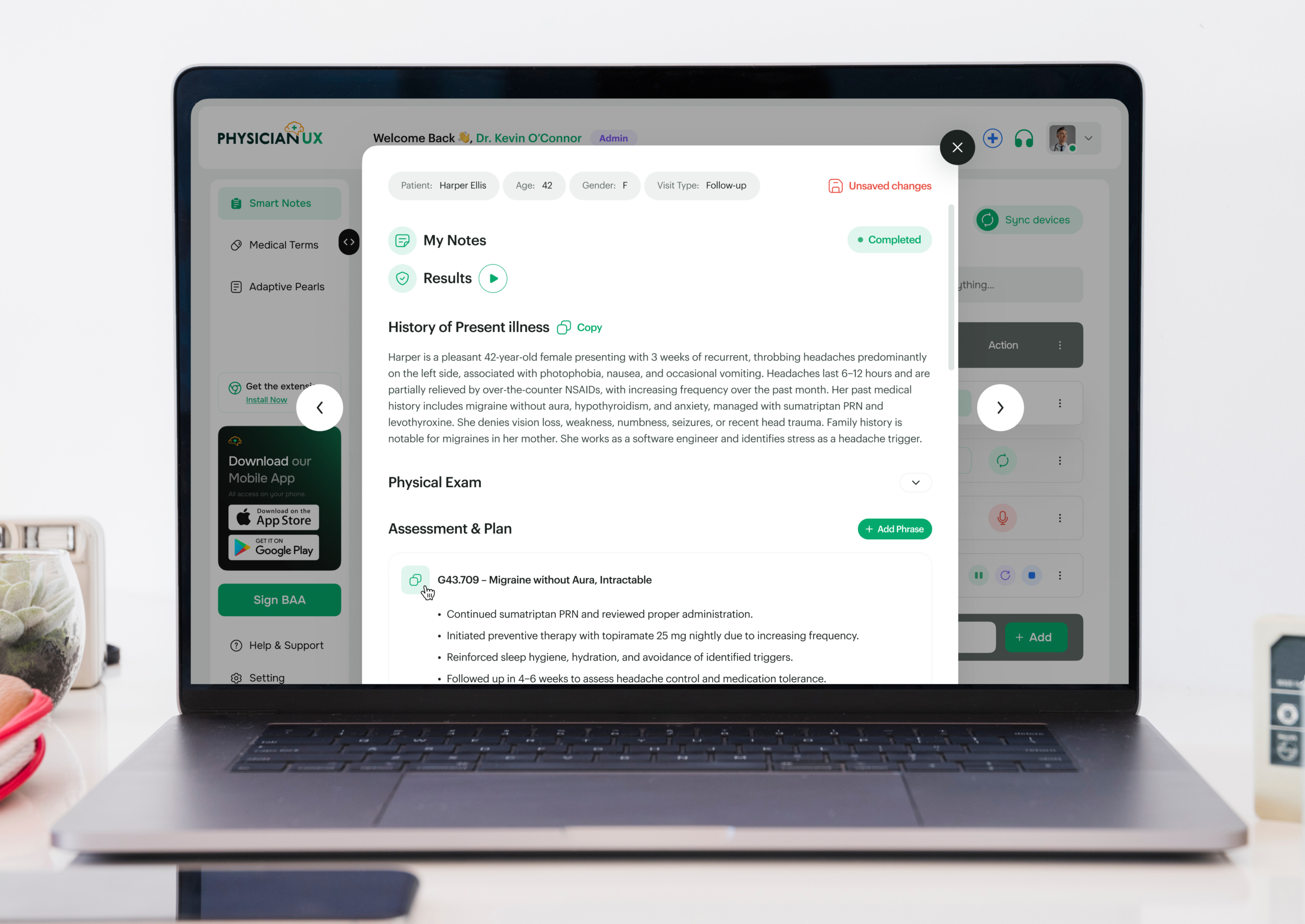
Neurology is defined by nuance — subtle exam findings, evolving symptoms, chronic disease trajectories, and acute neurologic events. What’s absent can matter as much as what’s present, and clinical reasoning often unfolds over time. Physician UX was designed to support this way of thinking, capturing conversations and producing notes that reflect how neurologists actually reason and manage care.
If you practice Neurology, you already know that notes often take longer than the visit itself. Neurological exams, cognitive assessments, imaging reviews, and ongoing management planning must be captured accurately — all while documentation requirements remain detailed, structured, and legally essential.
You’re capturing:
All while maintaining attention to subtle clinical changes — something no rigid template can fully support.
Neurology visits often require synthesizing multiple data sources, documenting complex findings, and planning multi-step management strategies. By the time you reconcile exams, labs, imaging, and treatment plans, the next patient is already waiting.
The cognitive load is high. Missed details can affect diagnosis, treatment outcomes, and continuity. Extended documentation hours accelerate clinician fatigue and burnout.
Physician UX lifts the documentation burden — without interrupting your workflow. It listens and structures notes in real time, supporting the precise and complex rhythm of Neurology care.
Dr. Kim, a neurologist in a busy outpatient clinic, begins her day with a mix of acute neurological complaints, chronic condition follow-ups, and cognitive assessments.
Typically, she would be mentally juggling imaging reviews, neurological exams, medication management, and therapy coordination — all while remaining attentive to each patient.
Today, Physician UX is listening in the background.
During her first visit, the platform structures a nuanced HPI based on symptom onset, neurological deficits, cognitive function, and prior imaging. By the end of the conversation, her note already includes an aligned assessment and plan — with tasks queued for labs, imaging, and specialist referrals.
Her second patient requires complex management of a neurodegenerative condition. Physician UX identifies key elements, surfaces pearls for treatment adjustments, and organizes tasks — all without slowing the encounter.
By mid-morning, Dr. Kim notices something rare: she is fully present with patients, not mentally reconstructing notes between visits.
Documentation that would normally extend into evenings is already complete. Tasks are organized, follow-ups mapped, and the burden of manual charting lifted. She can focus on neurological assessment, therapy planning, and patient counseling.
What used to feel like constant triage now feels like practicing Neurology at full capacity.
When charting becomes lighter and less intrusive, patient care transforms. Physician UX ensures notes are accurate, timely, and aligned with best practices — freeing cognitive bandwidth for critical neurological decision-making and patient-centered care.
Better notes also mean safer care:
In a specialty defined by precision, subtle findings, and ongoing assessment, clarity isn’t optional — it’s essential.
Join the clinicians who’ve upgraded their workflow — and feel the difference for yourself.