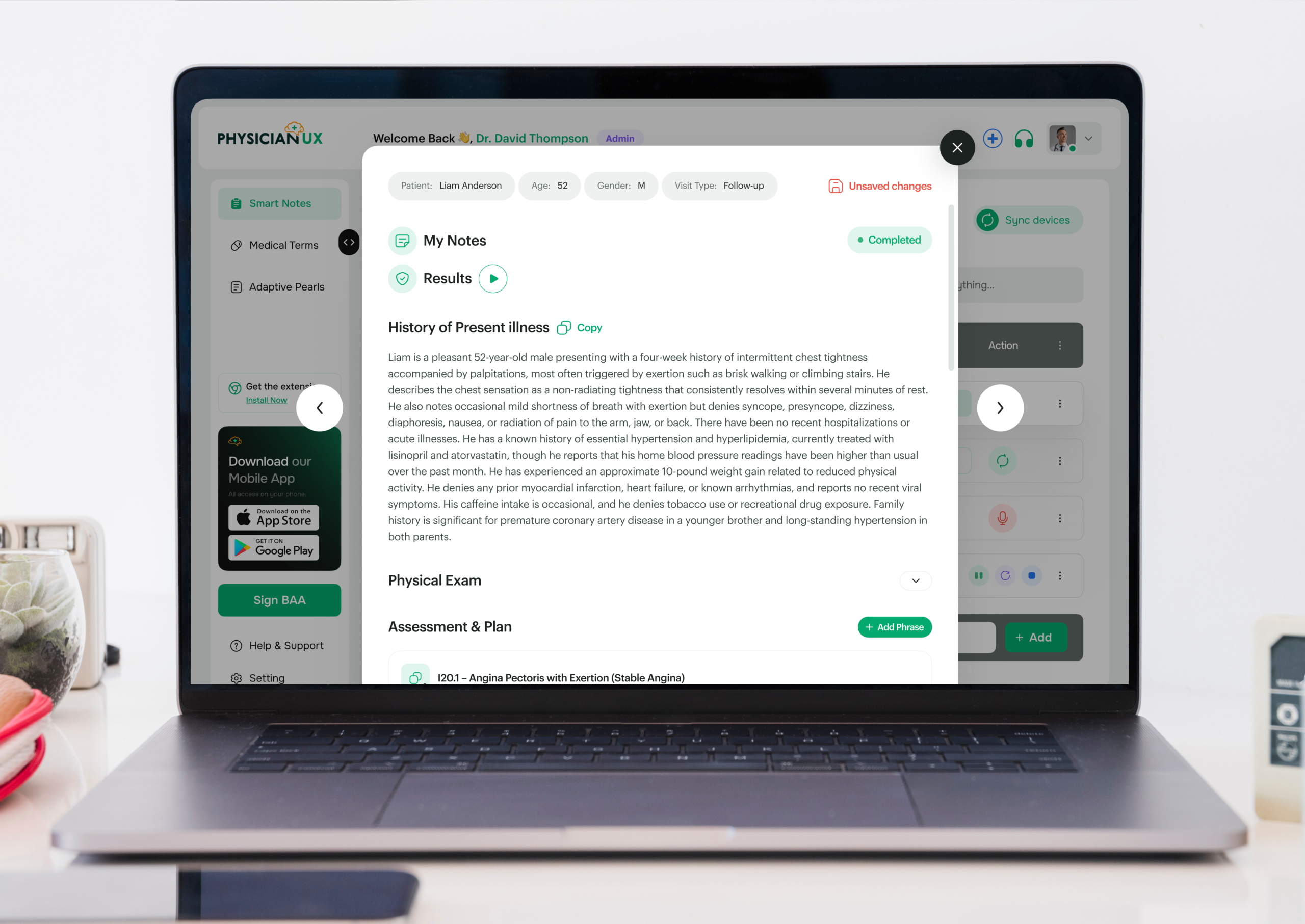
Built Around How Cardiologists Think
Cardiology is practiced through patterns — symptoms, risk factors, lab trends, imaging, and longitudinal decision-making that evolve over time. Each detail informs risk, diagnosis, and management. Physician UX was designed to follow that clinical reasoning, capturing conversations and transforming them into notes that reflect how cardiologists actually think and manage care in real time.
The Documentation Burden in Cardiology
If you practice Cardiology, you already know the frustrating reality: capturing a patient’s story takes longer than the visit itself. Chest pain is never just “chest pain.” Dyspnea, palpitations, edema, fatigue — the conversation branches into differential risks, comorbidities, hemodynamics, medications, and longitudinal trends. Meanwhile, the compliance expectations are high and unforgiving.
You’re documenting details like:
- Symptom quality, timing, triggers, and functional classification
- Medication adherence, intolerance patterns, and polypharmacy risks
- ECG interpretations, echocardiogram findings, and imaging impressions
- Risk scoring for ACS, heart failure, arrhythmias, and anticoagulation
- Chronic disease tracking: CAD, HF, AFib, hypertension, dyslipidemia
- Care coordination across primary care, EP, CT surgery, and imaging
All while staying present with patients who often arrive anxious, overwhelmed, or managing multiple conditions at once.
New patient intakes can stretch to 30–60 minutes, and follow-ups still require documenting vitals, symptom progression, functional status, lab trends, remote monitoring data, medication adjustments, and risk counseling. Reviewing imaging, ordering stress tests or echos, updating anticoagulation plans, and preparing referrals all add more cognitive load.
It’s not just time-consuming — it’s mentally taxing. Missed details can lead to care gaps or safety risks. And when documentation pushes into evenings or weekends, burnout isn’t far behind.
Where Physician UX Fits Into a Cardiologist’s Day
Physician UX lightens the load by following your clinical reasoning and documenting the full cardiology workflow — without slowing you down. It adapts to the way cardiology visits naturally unfold.
- Automatic visit capture that recognizes chest pain descriptions, dyspnea patterns, edema changes, palpitations, syncope, and functional status updates.
- Specialty-tuned SOAP notes that accurately reflect risk stratification, cardiac imaging details, guideline-based plans, and chronic disease management.
- Real-time Clinical Pearls surfaced during the visit — including guideline reminders for ACS, HF management, AFib anticoagulation, hypertension, lipid therapy, and imaging follow-up.
- Smart Phrases for chest pain workups, AFib rate/rhythm control, HF optimization, CAD secondary prevention, and hypertension adjustments.
- Automatic task generation for stress tests, echos, Holter monitors, medication titration follow-ups, anticoagulation checks, and lab monitoring.
- Clear referral summaries to EP, CT surgery, nephrology, sleep medicine, and imaging services.
- Reduced cognitive load so you can focus on risk interpretation, clinical decision-making, and patient reassurance — not clicking boxes.
A Real Clinic Day, Reimagined
How a Busy Cardiology Session Turns Manageable
Dr. Chen, a general cardiologist, starts her day with a marathon: chest pain evaluations, AFib management, chronic heart failure follow-ups, and a pre-op clearance squeezed into the schedule.
Normally she juggles symptom tracking, medication adjustments, imaging interpretation, and risk scoring mentally while racing through the EMR. Even with efficient workflows, the documentation backlog grows by the hour.
Today, Physician UX is running quietly in the background.
During her first patient — a woman with progressive dyspnea — Physician UX structures a detailed HPI from the conversation: exertional symptoms, orthopnea, edema, weight changes, medication adherence, sodium intake, and prior imaging. By the end of the visit, her note already includes a coherent assessment and guideline-aligned plan with tasks queued automatically for a BNP, echo, and medication titration follow-up.
Her next patient arrives with new palpitations and anxiety. As she explores triggers, frequency, and associated symptoms, the platform organizes the rhythm-focused differential and surfaces pearls on rate vs rhythm control strategies — supportive, relevant, not generic.
Halfway through clinic, she realizes she’s no longer behind. Her notes are complete, her tasks are organized, and her mind feels clearer — not cluttered.
By the afternoon, even her pre-op clearance is seamless: the platform captures surgical risk factors, functional assessment, medication considerations, and cardiac history, producing a clean summary ready to share.
What used to spill into after-hours work now finishes before lunch — without sacrificing accuracy or depth.
Better Documentation → Better Cardiac Care
In Cardiology, clarity and precision directly impact patient outcomes. When documentation becomes lighter and more automated, you gain the bandwidth to focus on what matters most: risk interpretation, patient education, and timely interventions.
Improved notes mean safer, more predictable care:
- Accurate tracking of symptoms, risk scores, vitals, and functional status
- Reliable documentation of imaging, ECGs, and medication changes
- Automated reminders for guideline-based follow-ups and monitoring
- More cohesive communication across EP, CT surgery, primary care, and imaging
- Real-time insights that support evidence-based cardiac decisions
When cognitive load decreases, clinical judgment sharpens — and patients feel the difference.